Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).
Patients admitted to Kingston Health Sciences Centre (KHSC) for the behavioural and psychiatric symptoms of dementia are benefiting from four new rooms and care dedicated to their unique needs.
“Being in the hospital can be confusing and stressful for people with dementia,” says Janet Obre, a nurse practitioner in KHSC’s Mental Health and Addiction program. “The surroundings are unfamiliar, everything looks the same, and the environment is often noisy and busy.”
While no one likes being hospitalized, the negative responses people with dementia may experience can lead to poor outcomes such as appetite loss, inability to perform daily activities, anxiety, wandering, resistance to care, withdrawal and longer hospital stays.
To lessen these effects, KHSC teams took an enhanced person-centred approach to care, supported by changes to the physical environment and care plans.
A strategic shift toward dementia-friendly care
Earlier this year, and after several months of planning, a multi-level strategy to address the complex needs of patients became a reality, thanks to a generous $27,200 donation from the Masons of Frontenac District, made through the University Hospitals Kingston Foundation.

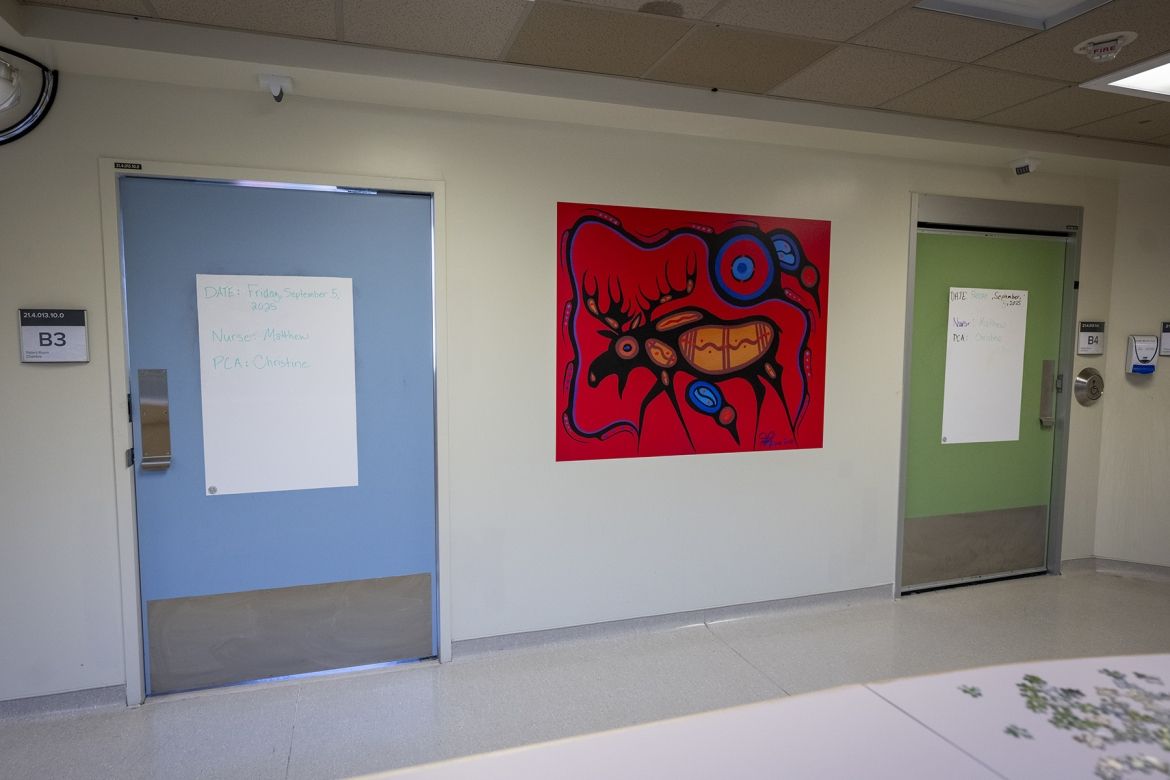
The new rooms are designed for patients who are medically stable but need hospitalization for a sudden state of heightened disorientation, serious behavioural changes, or to receive a higher level of psychiatric care that can’t be provided elsewhere.
Thoughtful changes to the hospital environment
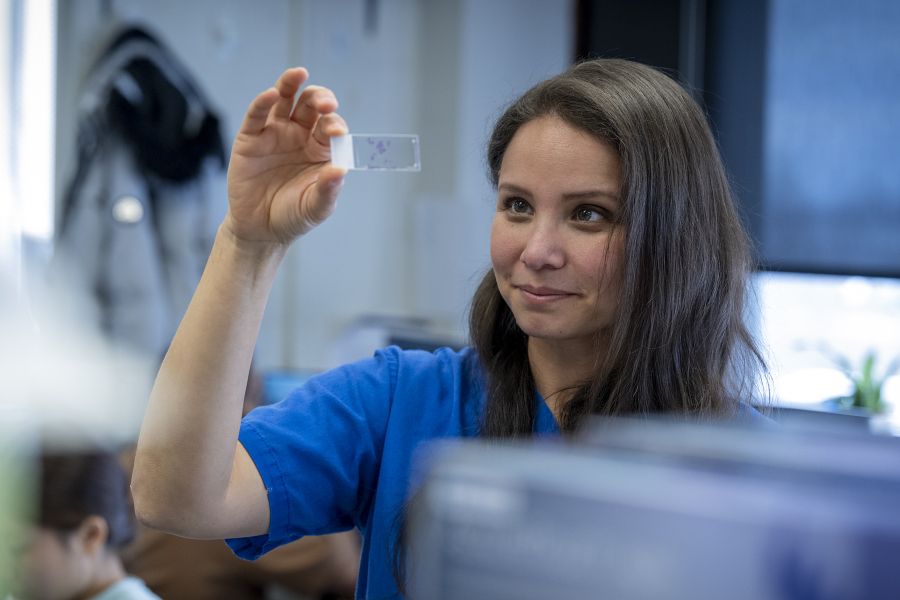
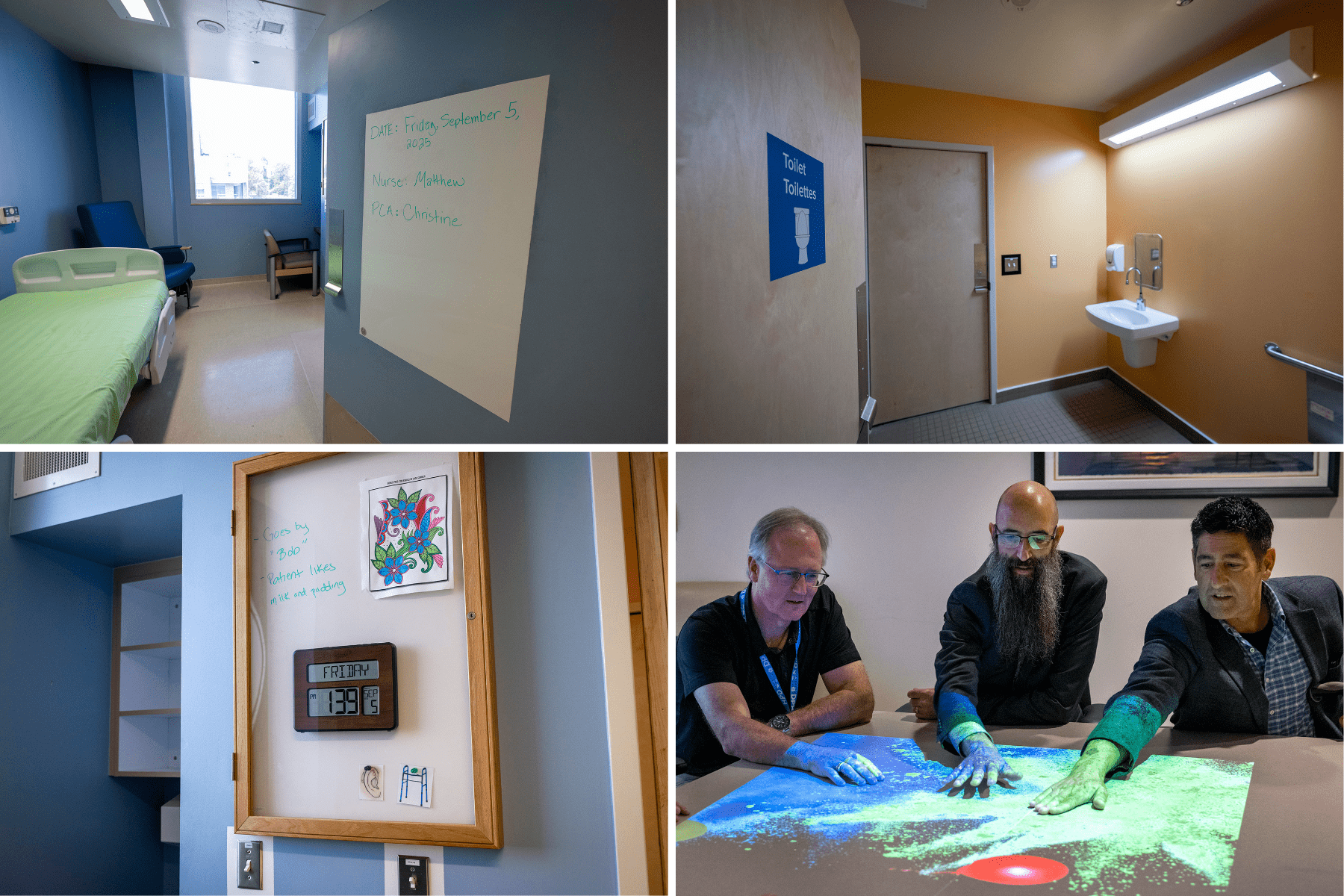
There is a lot less ‘hospital beige’ in these new psychiatric rooms dedicated to dementia care. Paint colours were chosen from a specific ‘dementia palette,’ as colour therapy is used to help promote desired emotional and physical states and makes it easier to find their way around the room. Walls and doors are painted green or blue, and the bathrooms are bright peach. Light switches are outlined in contrasting colours.
Night lighting installed lower to the ground and motion-activated lights in the bathrooms help them navigate safely and reduce sleep disruption.
In addition to colour and light, chairs that glide and large displays showing the time and date are also helping to reduce confusion and agitation for patients.
Personalized care that goes beyond the diagnosis
“When developing care plans, individual needs, preferences and life experiences are all considered to promote well-being and minimize distress,” says Obre, who was instrumental in bringing sensory light technology called the Happiness Programme to KHSC.
It’s a portable collection of interactive light games proven effective for people with cognitive challenges. Programming can be projected onto any surface, and it offers something for almost everyone, from painting pictures and brushing leaves to fishing and popping bubbles to playing tennis.

“The technology has enabled patients, families and staff to share engaging, meaningful moments that weren’t available before,” added Obre.
Patients and families are also involved in completing “All About Me” boards in patients’ rooms that help make their personal likes and activities known to care teams.
Knowing simple things like what cheers them up, a nickname, favourite music, if they have a pet, or use any aids at home, such as glasses or dentures, sends a strong message about caring for the whole person. This helps staff connect more deeply with patients, building trust and enabling more compassionate care.
By combining thoughtful design with individualized attention and by recognizing that dementia affects more than memory, KHSC care teams are helping to improve quality of life for vulnerable hospital patients with psychiatric symptoms.